Common Questions About Trigger Finger
What is it?
Trigger finger (also known as stenosing tenosynovitis) is a condition in which one experiences pain and swelling over the base of the thumb or finger. This is associated with a jerking, snapping or clicking when one extends the affected digit from a fully clenched position, much like how the trigger of a gun clicks when one pulls on it to fire, hence the name “trigger finger”. This happens due to a disparity of the size of the flexor tendon with its surrounding retinacular sheath of the affected digit. This is most common at the A1 pulley region. It is caused by a swelling of the flexor tendon synovium, which can be felt as a nodule, and/or thickening of the retinacular pulley. The passage of this tendon swelling into a tight sheath results in the triggering phenomenon. In severe cases, one may not even be able to fully flex the finger due to worsened tendon swelling or tightening of the sheath.
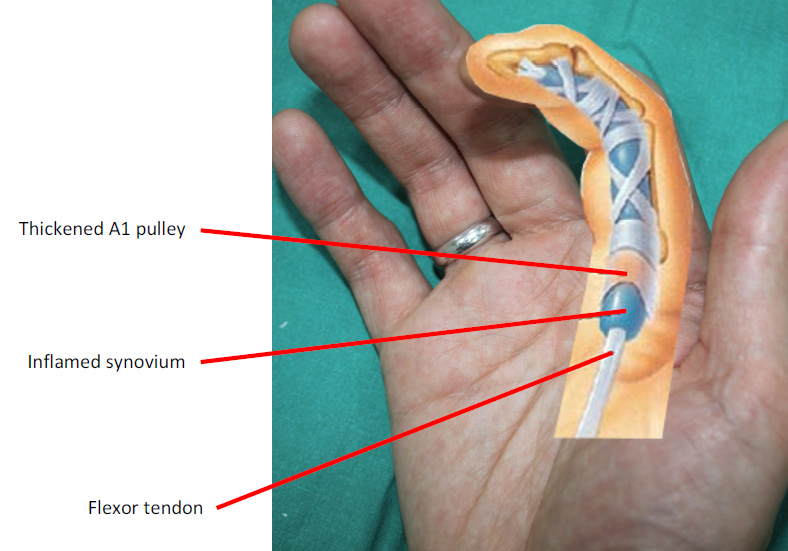
Figure 1. Right index finger demonstrating an inflamed
tendon with thickening of the A1 pulley.
Who gets this and why?
Trigger finger is commonly associated with age, existing medical conditions such as diabetes mellitus, rheumatoid arthritis and gout. However, most cases of trigger finger are idiopathic. It is believed constant or repetitive overuse of the fingers cause accumulated wear-and-tear at the interface between the flexor tendon and the A1 pulley, resulting in the swelling and inflammation that lead to triggering and pain.
What are the treatment options for trigger finger?
To determine the appropriate treatment modality for trigger finger, a qualified Hand Surgeon will firstly perform a thorough assessment by taking a detailed history and grading the severity of the trigger finger by careful clinical examination. Grading of trigger finger is as follows:
- Grade I – There is evidence of inflammation at the A1 pulley region of the affected digit, but no demonstrable triggering is noted.
- Grade II – There is evidence of inflammation at the A1 pulley region of the affected digit with demonstrable triggering when the patient is asked to extend the digit from a fully flexed position.
- Grade IIIA – Same as grade II, but in addition, the patient is unable to fully extend the digit actively as it gets locked in a flexed position and is achieved only with assistance of the other hand.
- Grade IIIB – The patient is unable to fully flex the digit due to the severe inflammation at the A1 pulley region.
- Grade IV – There is a fixed flexion deformity at the proximal interphalangeal joint due to longstanding inflammation.
There are 3 ways to treat trigger finger.
- Non-surgical, non-invasive: This involves a course of oral non-steroidal anti- inflammatory medication, hand therapy, splinting and activity modification. Generally, this is recommended only in first-time trigger finger sufferers with grade I or early grade II disease.
- Non-surgical, invasive: This involves an injection directly into the flexor tendon sheath of a mixture containing a local anaesthetic agent and a corticosteroid preparation. This resolves the inflammation at the A1 pulley site and relieves the trigger finger. This effect may or may not be longlasting and recurrence is always a possibility. Repeatedinjections should not be attempted. Hand Surgeons advocate a maximum of 2 injections to an affected digit, except the little finger, which should be limited to only 1. The belief is that corticosteroids weaken the tendon and can result in atraumatic tendon rupture if subjected to repeated injections. This treatment is recommended for failed trial of non-invasive treatment and grade II or III triggers.
- Surgical intervention: This involves releasing the A1 pulley, pre-annular pulley and even part of the A2 pulley if necessary through a small skin incision made at the base of the digit (Figure 2). It is rare for trigger finger to recur after surgical release. For grade IV trigger finger, manipulation of the proximal interphalangeal joint is done at the same sitting to reduce the flexion deformity. In severe cases, a formal flexion contracture release is performed through a separate incision.
Why see a Hand Surgeon for trigger finger?
Hand Surgeons have vast experience in managing conditions of the fingers, hands and wrist exclusively. Therefore, they are well-equipped with skills and knowledge to handle all grades of trigger finger. Supervised hand therapy and specialty splints, such as a figure-of-eight splint(Figure 3) used in the treatment of early grade trigger fingers are prescribed in Hand Surgery Centres with in-house hand occupational therapists. Hand Surgeons are trained to give accurate intra-thecal flexor sheath injections to maximise the possibility of cure and minimise the chance of recurrence. If surgery is indicated, Hand Surgeons perform the most meticulous operation to release the trigger, and, if necessary, correct the flexion deformity of the proximal interphalangeal joint through a formal contracture release via a Bruner incision. Skin incisions are made within the natural crease lines to achieve a virtually scar-free result (Figure 4)

Figure 3. A figure-of-eight splint.

Figure 4. This patient underwent trigger release surgery
for the left ring and little fingers. Resulting scars circled.
Quick Find
Have a Question?
Send us an email or enquire directly at the respective clinics for prompt assistance.

